Open Enrollment, Annual Enrollment, Renewal Time, no matter what you call it there is considerable planning, negotiating, education, organization… and likely a little anxiety during this season! For companies with plans that begin January 1, this time period falls during the 4th quarter of the year (whether your enrollment date falls here or not, the process is the same). There are certain steps that we have identified to help guide your company through this process.
A. Plan Design Changes
ACA Affordability Standard
 Most medical plans are ACA compliant, meaning they meet certain benefits and dollar maximums as established by the Affordable Care Act. The impact varies depending upon the size of your company. Companies that are considered an applicable larger employer (ALE) are required to offer affordable, minimum value health coverage to their full-time employees (and dependent children) or risk paying a penalty. An ALE is a company that has 50 or more full-time equivalent employees. This “employer mandate” or “pay or play” as it is often referred to, is the employer’s shared responsibility requirements.
Most medical plans are ACA compliant, meaning they meet certain benefits and dollar maximums as established by the Affordable Care Act. The impact varies depending upon the size of your company. Companies that are considered an applicable larger employer (ALE) are required to offer affordable, minimum value health coverage to their full-time employees (and dependent children) or risk paying a penalty. An ALE is a company that has 50 or more full-time equivalent employees. This “employer mandate” or “pay or play” as it is often referred to, is the employer’s shared responsibility requirements.
An Applicable Large Employer’s health plan is affordable if the cost to the employee does not exceed a certain percentage of their income. This amount is set each year by the IRS. For the plan year 2022, the adjusted percentage is 9.61% and will decrease to 9.12% for plan years that begin on or after January 1, 2023. This is the most substantial decrease since these rules were implemented and are the lowest that this percentage has ever been set at 0.38% below the statutory affordability percentage of 9.5%. This will lead many employers to assume a higher cost of health insurance for the employee contribution to meet this affordability test.
For employers with less than 50 full-time eligible employees (while the employer is not required to provide health insurance) the affordability testing will still play a role. If an employee pays more than 9.12% of their household income for a plan that begins January 1, 2023, they may be eligible to purchase individual coverage on the Marketplace and perhaps be eligible for a subsidy as well. However, if the employer’s plan is affordable then their employees are not eligible for subsidized coverage.
Out-of-Pocket Maximum
 Under the Affordable Care Act, health plans (plans that are non-grandfathered) are subject to limits on cost sharing for essential health benefits (EHB). The annual total enrollee cost sharing for EHB for plan years beginning on or after January 1, 2023, is $9,100 for self-only coverage and $18,200 for family coverage. Be sure to review your plan’s out-of-pocket maximum.
Under the Affordable Care Act, health plans (plans that are non-grandfathered) are subject to limits on cost sharing for essential health benefits (EHB). The annual total enrollee cost sharing for EHB for plan years beginning on or after January 1, 2023, is $9,100 for self-only coverage and $18,200 for family coverage. Be sure to review your plan’s out-of-pocket maximum.
If you have a high deductible health plan (HDHP) compatible with a health savings account (HSA) the out-of-pocket maximums are lower. For the 2023 plan years, the out-of-pocket maximum limit for HDHPs is $7,500 for self-only coverage and $15,000 for family coverage.
Preventive Care Benefits
The ACA requires certain preventive health services to be covered at no cost for non-grandfathered health plans. Health plans are required to adjust their first-dollar coverage of preventive care services based on the latest recommended preventive care services without any cost sharing.
Two websites with more detailed information on coverage requirements: www.HealthCare.gov and U.S. Preventive Services Task Force.
Health FSA Contributions
The IRS imposes a dollar limit on employees’ salary reduction contributions to a health flexible spending account (FSA) offered under a Section 125 plan. An employer may set their own dollar limit on employees’ salary reduction contributions to a health FSA if the employer’s limit does not exceed the ACA’s maximum limit in effect for that plan year. While the 2023 health FSA limit has not yet been released, it is projected to be $3,050 (a $300 increase from $2,850 in 2022).
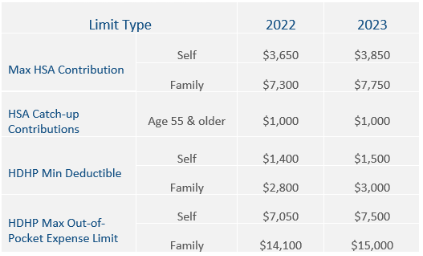
HDHP and HSA Limits for 2023
The IRS limits for HSA contributions, HDHP minimum deductible, and HDHP maximum out-of-pocket expenses increase for 2023. The HSA contribution limits will increase effective January 1, 2023, while the HDHP out-of-pocket limit will increase for plan years beginning on January 1, 2023.
B. ACA Disclosure Requirements
Summary of Benefits and Coverage
Health plans and health insurance issuers are required by the ACA to provide a Summary of Benefits and Coverage (SBC) to participants and beneficiaries who enroll or reenroll during an open enrollment period (including those newly eligible for coverage and special enrollees).
The Departments of Labor and Health and Human Services have established the SBC template and required materials which are updated annually. The 2023 template is required as plans renew from January 1st forward through 2023. This SBC must be given annually 30 days before the new plan year (whether or not the medical plan design is changing).
Grandfathered Plan Notice
If you have a grandfathered health plan, make sure to include information about the plan’s grandfathered status in your employee materials (SPD, open enrollment materials, benefit booklets, etc.).
Notice of Patient Protections
 Non-grandfathered group health plans and issuers that require the designation of a participating primary care provider must permit each participant, beneficiary, and enrollee to designate any available participating primary care provider, as required by the ACA. Plans and issuers that provide obstetrical/gynecological care and require a designation of a participating primary care provider may not require preauthorization or referral for obstetrical/gynecological care. Notice of these patient protections must be provided whenever the SPD or similar benefit descriptions are provided to a participant.
Non-grandfathered group health plans and issuers that require the designation of a participating primary care provider must permit each participant, beneficiary, and enrollee to designate any available participating primary care provider, as required by the ACA. Plans and issuers that provide obstetrical/gynecological care and require a designation of a participating primary care provider may not require preauthorization or referral for obstetrical/gynecological care. Notice of these patient protections must be provided whenever the SPD or similar benefit descriptions are provided to a participant.
C. Other Notices
Other annual notices that we recommend health plan sponsors provide to their employees annually include:
- Initial COBRA Notice
- Notice of HIPAA Special Enrollment Rights
- Summary Plan Description
- HIPAA Privacy Notice
- Annual CHIPRA Notice
- WHCRA Notice
- Medicare Part D Notices
- Summary Annual Report
- Michelle’s Law Notice
- HIPAA Opt-out for Self-funded, Non-federal Governmental Plans
- Wellness Program Notice
- HIPAA Wellness Program Notice
- Americans with Disabilities Act (ADA) Wellness Program Notice
Recognizing the complexities of the open enrollment period, we are committed to making this required course of action simple for our clients and their employees. Our processes, employer materials, and employee education are specific to each client’s needs.


