Sponsors of self-funded ERISA plans bear fiduciary responsibilities toward plan participants, including the duty to thoroughly review claims and engage effectively with participants regarding claim denials. eBen has a very specific and well-outlined approach to not only protect the ERISA plan sponsor, but also to clearly and easily identify the process for the plan participants.
Appeals
When a claimant receives notification of an Adverse Benefit Determination, the claimant generally has 180 days following receipt of the notification in which to file a written request for an appeal of the decision. However, for Concurrent Care Claims, the claimant must file the appeal prior to the scheduled reduction or termination of treatment. For a claim based on rescission of coverage, the claimant must file the appeal within 30 days. A claimant may submit written comments, documents, records, and other information relating to the claim.
If the claimant so requests, he or she will be provided, free of charge, reasonable access to, and copies of, all documents, records, and other information relevant to the claim. The Plan Administrator shall provide the claimant, as soon as possible and sufficiently in advance of the time within which a final determination on appeal is required to allow the claimant time to respond, any new or additional evidence that is relied upon, considered or generated by or at the direction of the plan. This evidence shall be provided free of charge.
A document, record, or other information shall be considered relevant to a claim if it:
- was relied upon in making the benefit determination;
- was submitted, considered, or generated in the course of making the benefit determination, without regard to whether it was relied upon in making the benefit determination;
- demonstrated compliance with the administrative processes and safeguards designed to ensure and to verify that benefit determinations are made in accordance with plan documents and plan provisions have been applied consistently with respect to all claimants; or
- constituted a statement of policy or guidance with respect to the plan concerning the denied treatment option or benefit.
 The period of time within which a benefit determination on appeal is required to be made shall begin at the time an appeal is filed in writing in accordance with the procedures of the plan. This timing is without regard to whether all the necessary information accompanies the filing.
The period of time within which a benefit determination on appeal is required to be made shall begin at the time an appeal is filed in writing in accordance with the procedures of the plan. This timing is without regard to whether all the necessary information accompanies the filing.
Before the Plan Administrator issues its Final Adverse Benefit Determination based on a new or additional rationale, the claimant must be provided, free of charge, with a copy of the rationale. The rationale must be provided as soon as possible and sufficiently in advance of the time within which a final determination on appeal is required to allow the claimant time to respond. If it is impossible under the circumstances to give the claimant a reasonable time to respond, the period for issuing the Final Adverse Benefit Determination will be delayed until the claimant has a reasonable opportunity to respond. After the claimant responds, or if the claimant fails to do so, the Plan Administrator will issue its Final Adverse Benefit Determination as soon as reasonably possible, taking into account the medical requirements.
The review shall take into account all comments, documents, records, and other information submitted by the claimant relating to the claim, without regard to whether such information was submitted or considered in the initial benefit determination. The review will not afford deference to the initial Adverse Benefit Determination and will be conducted by a fiduciary of the plan who is neither the individual who made the adverse determination nor a subordinate of that individual.
If the determination was based on a medical judgment, including determinations with regard to whether a particular treatment, drug, or other item is Experimental, Investigational, or not Medically Necessary or appropriate, the fiduciary shall consult with a health care professional who was not involved in the original benefit determination. This health care professional will have appropriate training and experience in the field of medicine involved in the medical judgment. Additionally, medical or vocational experts whose advice was obtained on behalf of the plan in connection with the initial determination will be identified.
- Information sufficient to allow the claimant to identify the claim involved (including date of service, the healthcare provider, and the claim amount, if applicable), and a statement that the diagnosis code and treatment code and their corresponding meanings will be provided to the claimant as soon as feasible upon request.
- The specific reason or reason for the adverse determination, including the denial code and its corresponding meaning, and a description of the plan’s standard, if any, that was used in denying the claim.
- Reference to the specific plan provisions on which the determination was based.
- A description of any additional materials or information necessary for the claimant to perfect the claim and an explanation of why such material or information is necessary.
- A description of the plan’s internal and external review procedures and the time limits applicable to such procedures. This will include a statement of the claimant’s right to bring a civil action under section 502 of ERISA following an Adverse Benefit Determination on review.
- A statement that the claimant is entitled to receive, upon request and free of charge, a reasonable access to, and copies of, all documents, records, and other information relevant to the claim.
- If the Adverse Benefit Determination was based on an internal rule, guideline, protocol, or other similar criterion, the specific rule, guideline, protocol, or criterion will be provided free of charge. If this is not practical, a statement will be included that such a rule, guideline, protocol, or criterion was relied upon in making the Adverse Benefit Determination and a copy will be provided free of charge to the claimant upon request.
- If the Adverse Benefit Determination is based on the Medical Necessity or Experimental or Investigational treatment or similar exclusion or limit, an explanation of the scientific or clinical judgment for the determination, applying the terms of the plan to the claimant’s medical circumstances, will be provided. If this is not practical, a statement will be included that such explanation will be provided free of charge, upon request.
- Information about the availability of and contact information for, any applicable office of health insurance consumer assistance or ombudsman established under applicable federal law to assist individuals with the internal claims and appeals and external review process. In addition, a statement that “You and your plan may have other voluntary alternative dispute resolution options, such as mediation. One way to find out what may be available is to contact your local U. S. Department of Labor Office.
If the claimant disagrees with the Adverse Benefit Determination on Appeal, he or she may file a request for a second level of appeal. This request must be made in writing within 180 days following receipt of the Adverse Benefit Determination on Appeal. The claimant may submit written comments, documents, records, and other information relating to the claim.
The second level of review will be conducted, and written notification of the decision, shall be made in accordance with all of the procedures that apply to the first level of review. If the claim is denied in whole or in part after this second level of appeal, the written notification describing the Adverse Benefit Determination is the Final Adverse Benefit Determination.
External Review Process
If a claimant receives a Final Adverse Benefit Determination under the plan’s internal claims and appeals procedures, he or she may request that the claim be reviewed under the plan’s external review process. This request must be filed in accordance with the applicable State external review process. Please contact the Plan Administrator for more details.
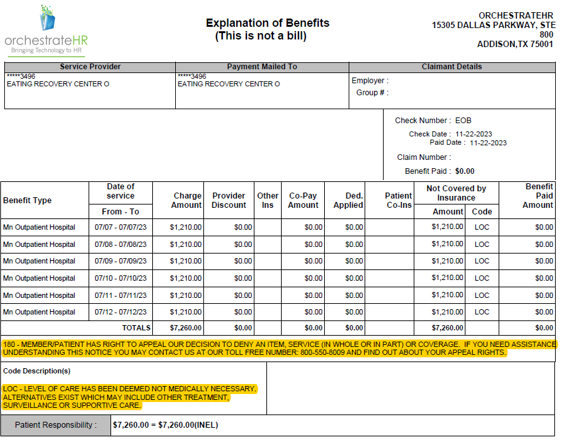
Explanation of Benefits
An Explanation of Benefits (EOB) is a document provided by they claims administrator to policyholders after a medical claim has been processed. The EOB outlines the details of the services rendered, the amount billed by the healthcare provider, the portion covered by the insurance company, any deductibles or co-payments, and the amount the policyholder may owe to the healthcare provider. It serves as a summary of the healthcare services received and the financial responsibilities associated with those services. EOBs are essential for policyholders to understand the costs associated with their medical care and to ensure accuracy in billing and insurance coverage.